Heel Pain Clinic
Active Health has a dedicated Heel Pain Clinic that provides specific treatment for heel pain including Plantar Fasciitis, Achilles Tendinopathy, Sever's (Heel Pain in Children), Bursitis & Heel Spurs.
Heel pain can be completely debilitating, it can stop you from exercising, walking without pain and just makes daily activities difficult. After all, we need our feet to carry us around everyday! Perhaps you can relate…
Heel pain can last for months and even years if not well managed or allowed to heal properly. The heel and its surrounding structures are engaged with every step so it can be difficult to live an active life when you are reminded of that pain every morning when you first get out of bed.
Experience The Difference
Active Health provides a unique multi-disciplinary approach to treating your heel pain. Our Podiatrists work closely with our team of Physiotherapists and Exercise Physiologists to get to know you, identify the true cause of your heel pain, build a treatment plan tailored to your needs & get you back to your active life sooner.
What to Expect
Combining the latest evidence based treatment techniques and 19 years of clinical experience treating Heel Pain, you will receive a personalised treatment plan that will outline your roadmap to recovery and keep you on track to reaching your goals.
In this plan you will:
Finally discover the what is causing your heel pain (it may not be what you think)
Identify & set your goals for treatment
Receive the latest evidence based treatments
Learn self-management exercises to relieve your pain at home
Leave with clarity and certainty about how you can be heel pain free
The best form of treatment is early intervention, so the sooner you seek treatment the greater chance of making a quick recovery.
We are here to help, if you have been suffering with Heel Pain make an appointment with our experienced Podiatrist to finally put an end to your heel pain!
What treatments do we offer
Active Health provides a number of treatments based on your assessment & specific needs. The primary goal is to identify the true cause of your injury, reduce pain and symptoms, then focus on increasing the capacity of the injured structure to improve strength & mobility to keep you active & prevent it from returning.
The latest evidenced based treatments offered at Active Health can include:
Foot Mobilistaion Therapy
Strengthening Exercises
Taping & Padding
Flexible Orthotics
Shockwave Therapy
Dry Needling
Massage
Mobility exercises
Footwear Education and Modifications
Gait Walking/Running Re-training
Activity Modification
Types of Heel Pain that we Treat
Any type of heel pain including the following conditions:
PLANTAR FASCIITIS
Do you wake up in the morning with a sharp pain in your heel? Does this pain slowly improve as you take more steps? You may be suffering from Plantar Fasciitis.
What is Plantar Fasciitis?
Plantar Fasciitis, also known as Plantar Fasciopathy, is the most common condition that our Podiatrists see in the clinic. It is a soft tissue injury of the plantar fascia, a thick band of connective tissue on the bottom of your foot that helps to stabilise and support your foot when you walk, run and move.
What causes Plantar Fasciitis?
The plantar fascia plays a vital role in allowing the foot to absorb shock when we land and provide us with a rigid lever and elastic energy when we push off.
The cause of Plantar Fasciitis is multifactorial but is mostly related to an increase in load greater than the capacity of the plantar fascia tissue.
Some examples of an increase in load include:
Limited ankle range of motion
Increased activity
Foot Biomechanics - The way your foot functions during gait can increase load on the plantar fascia
Time spent on your feet at work
When the plantar fascia is overloaded it can become inflamed, thickened and degenerate. This repetitive tension and load can cause microtears in the plantar fascia at the insertion of the heel.
When is it mostly painful?
It can be mostly painful first thing in the morning or rising from sitting as the plantar fascia is at its shortest functional length at rest and pulls tight on the insertion of the heel when we stand. The pain can tend to improve once we hobble around for a short while as the plantar fascia becomes more elastic but returns with increased walking/load during the day.
How do we treat Plantar Fasciitis?
A quick Google search will show you that there is a wide range of treatments available for Plantar Fasciitis. It is important to seek a Health Professional & build a treatment plan that is best suited to your needs.
Our treatment plan for Plantar Fasciitis can be simplified into 3 main stages of rehab:
1. De-load
The first stage of treatment is focused on reducing pain and symptoms, this can be achieved by Decreasing load to the plantar fascia. Our goal at Active Health is to reduce load to the painful heel to encourage healing but still keep you moving. We can provide solutions to slightly modify your activities to decrease pain while we work on building the capacity of the plantar fascia and the supporting structures.
2. Re-load
Once your symptoms and pain levels have started to improve, we focus on improving the strength and capacity of the plantar fascia and the surrounding muscles by gradually Re-introducing load. The plantar fascia responds well if it is loaded in the right way at the right time. Our team at Active Health will work together to formulate a load management plan that keeps you active but still allows adequate time for healing.
The key areas that we work on include:
Ankle & Big Toe Mobility
Foot & Ankle Strengthening
Balance and and lower limb stability
3. Increase load
This stage of rehab focuses on progressively Increasing load to further strengthen the foot, ankle and lower limb. This will ensure a full return to activity, often stronger than you were pre-injury, to prevent it from returning and get you back doing what you love.
ACHILLES TENDINOPATHY
The Achilles Tendon is a remarkable structure that transmits forces from the calf muscle complex to the foot and ankle.
It is the largest and strongest tendon in the human body, for good reason as it has to withstand 12 x our body weight when running. Given the increased demand/load that is placed on the achilles tendon when active it is no wonder that we see a number of people with pain and dysfunction, commonly known as Achilles Tendinopathy.
What is Achilles Tendinopathy?
Achilles Tendinopathy is pain around the back of the heel most commonly seen in people that have had a sudden increase in their activity and/or load. For instance, those that have suddenly started running or returned to sport after a long spell.
There are 2 types of Achilles Tendinopathy based on the anatomic location of symptoms. The most common is Mid-Portion, which as the name suggests is pain of the mid-portion of the achilles tendon approximately 2-6cm above its insertion of the heel. The other is Insertional, which is pain located at the junction where the tendon attaches to the heel.
Pain can often present with morning stiffness when getting out of bed, or getting up from sitting and will increase with running or jumping. It can tend to “warm up” with activity and return when cooled down or the following day. The tendon may also appear swollen and thickened at the site of pain.
What causes Achilles Tendinopathy?
Common causes of Achilles Tendinopathy include a sudden increase in activity or training load, abrupt transition to minimalist shoes, reduced ankle range of motion and weak calf muscles.
How is it treated?
Treatment of Achilles Tendinopathy will be dependent on your assessment findings but mostly consists of temporarily modifying your training load, particularly energy storage and release exercises such as running, jumping and hopping. We will also incorporate a graduated strengthening program to ensure optimal healing and prevent it from happening again.
Appropriate calf muscle strength is key for managing achilles tendinopathy and therefore assessment of its function is important in the initial assessment. Active Health utilises a variety of tests to objectively assess calf function, including use of the state of the art AxIT System.
Active Health provides a number of treatment for Achilles injuries options including Shockwave Therapy, footwear modifications, dry needling, foot & ankle mobilisations, stretching, taping and orthotic therapy.
SEVERS
Heel pain is a common complaint in active children between the ages of 8-14 years of age. It is most likely a condition called Calcaneal Apophysitis, or more commonly known as Severs Disease.
What is Severs?
Severs is inflammation of the growth plate at the back of the heel where the achilles tendon attaches to the heel bone (Calcaneus).
Signs & Symptoms:
• Heel pain during or after physical activity
• Pain around the back of the heel bone
• Limping or calf stiffness first thing in the morning
• Walking on toes or avoiding pressure on heels
What causes Severs?
Severs is thought to occur because the growth where the achilles tendon attaches to the bone (the apophysis) is ‘active’. This means it is beginning to change from cartilage to bone.
Severs can be caused by an increase in activity during the early growth spurts of puberty. Particularly activities that involve running, jumping or change in directions. These activities can increase the load through the calf muscles causing inflammation and irritation of the growth plate on the heel.
How can we help?
Severs is a self-limiting condition, which means symptoms will resolve over time as the growth plate becomes less active. However, the pain associated with Severs can be debilitating and can impact on a child’s participation in sport and activities.
Treatment is aimed at reducing pain and symptoms so that they can continue to be active. Load management and activity modification is important in the early stages to reduce pain and flare ups. This can be achieved by modifying their activity or training, reducing load to the heel by using taping, heel lifts, orthotics or footwear modifications.
The growth plate can take 2 or more years to mature so it is important to seek a health professional to learn how to manage the flare ups, which can be triggered by growth spurts, changes in activities and intensity, and changes in footwear.
BURSITIS
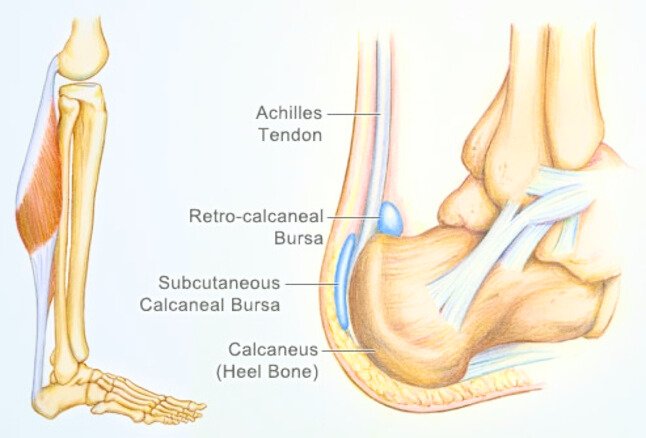
Bursitis is a painful condition that affects the small fluid-filled sacs, called Bursae, that cushion the bones, tendons and muscles. Bursae act to reduce friction and assist in the movement of tendons over bony surfaces.
What is Bursitis?
Bursitis occurs when bursae become irritated and inflamed due to repetitive movements.
Retrocalcaneal Bursitis is a common heel bursitis involving inflammation of the bursae located between the heel bone (calcaneus) and the Achilles Tendon.
Subcutaneous Calcaneal Bursitis is another heel bursitis located between the heel bone and the subcutaneous tissue. This bursitis usually presents with pain when getting out of bed in the morning and returns with increased walking during the day.
What causes Bursitis?
Inflammation of the heel bursae is most commonly caused by repetitive movements or overuse that cause irritation to the bursae. The condition can be aggravated by pressure, such as tight fitting shoes or due to an impingement on a bony growth on the back of the heel, known as a Haglund’s Deformity.
Signs & Symptoms:
Pain at the back of the heel with localised swelling and redness
Pain may get worse when rising on toes
Stiffness at the heel in the morning
Increased pain with activities that load the calf muscle
How do we treat it?
The aim of treatment during the acute phase is to reduce pain and swelling. This can be achieved by reducing excessive load to the achilles tendon including the use of heel raises, footwear education, anti–inflammatories and activity modification.
Gradual progressive stretching and strengthening of the calf can help to relieve impingement of the bursae and prevent flare ups.
HEEL SPUR
If you have suffered with heel pain for a long period of time, you may have developed a heel spur.
However… the heel spur is unlikely to be the cause of your heel pain.
What is a Heel Spur?
A heel spur is a bony prominence that extends from the heel bone (Calcaneus).
Heel spurs most commonly form underneath the heel at the insertion of the plantar fascia. They are usually associated with a tight plantar fascia or Plantar Fasciitis.
They can also develop on the back of the heel bone at the insertion of the achilles tendon. They are usually associated with a prolonged period of Achilles Tendinopathy, calf muscle tightness or ill-fitting shoes.
What causes a heel spur?
Bone spurs are caused by abnormal bone growth. When there is constant irritation and stress on the bone for greater than 6-8 weeks, the cells responsible for bone growth are stimulated to produce calcium deposits to protect the bone from injury. As the calcium deposits build up over time a spur shaped deformity forms, which can be seen below on X-ray.
Imaging studies have shown that heel spurs do not always cause heel pain. The heel spur is often a side effect of the real underlying cause of your heel pain, such as Plantar Fasciitis or Achilles Tendinopathy. By treating these underlying conditions symptoms associated with the heel spur often resolve.
Signs & Symptoms:
Pinpoint sharp, stabbing pain in the heel on rising first thing in the morning
Dull ache in the heel towards the end of the day
Stiffness in the ankle and calf
Hard painful lump
How do you treat a heel spur?
The first step in treating heel spurs is to identify the true cause of your heel pain. Most often this will involve the plantar fascia, achilles tendon or other structure surrounding the heel including the fat pad.
Depending on the cause of your heel spur, treatment will be tailored specifically to the diagnosis. Commonly heel spur treatments include:
Strengthening & Stretching exercises - To reduce tensile stress at the insertion of the tendon and strengthen the supporting muscles
Orthotics - To improve foot function and reduce load to the painful area
Footwear Modifications - Heel cups to cushion the heel spur and education on the most appropriate footwear for your feet
Taping and padding - Reduce pressure on painful areas
Treating the surrounding soft tissue structures will often resolve all pain and symptoms. In rare cases surgery may be required to remove the spur if conservative treatment fails to relieve pain.